Designing a minimum viable genetic testing service for the NHS.
With the publication of NICE guidance that stipulated stroke patients should receive a genetic test to inform their prescribing, the impetus was there to pilot a genetic testing service in high volume, acute care for the first time.
This project was commissioned by NHS England and delivered in partnership with Videha Sharma from The University of Manchester via the North West Genomic Medicine Service Alliance.
Pharmacogenetics, or ‘personalised medicine’ has the potential to revolutionise prescribing and save the NHS millions. It involves testing people’s genes to ensure they are prescribed the right medication for them. While the scientific research on this is extensive, use of this kind of genetic testing in routine care is currently limited to cancer and rare disease. Previously we explored how this testing could be integrated at a primary care level.

Joining up strategy and service design and delivery.
The publication of NICE guidance provided the need for the NHS to accelerate the move towards integrating genetic testing into routine care, this time in a hospital care setting, both at a strategic and a front-line service delivery level. This project provided a rare opportunity for one to inform the other.
While NHS England were working on the wider strategy for rolling out genetic testing across the country, they commissioned us to lead the delivery of a pilot in three hospitals to design and test a minimum viable lab based testing service.
Designing a real service, not a pilot project.
We worked with the clinical teams in all three hospitals to design a new end-to-end service that involved multiple clinical staff including consultants, junior doctors, phlebotomists, local lab staff and national lab staff.
As is usual in pilot studies in the NHS, the inclination was there to wrap the project in cotton wool to ensure it went well. What we did was encourage the clinical teams to move towards designing and delivering a service that would work in a routine care setting, a service that wasn’t perfect but one we could learn from and adapt to ensure the best experience for staff and patients. This involved integrating with existing processes and services like local IT systems, phlebotomy and the on-site lab.

Navigating constraints.
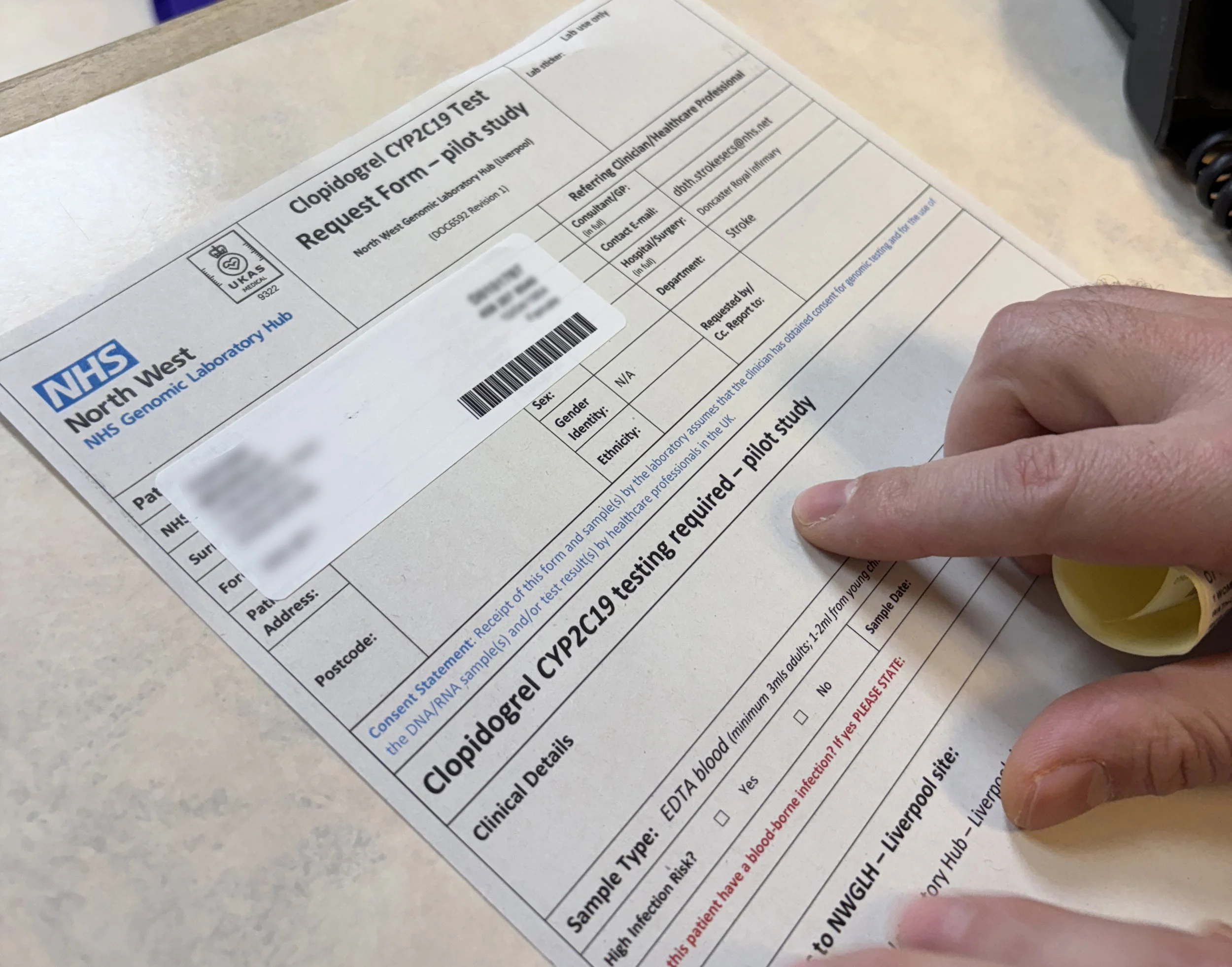
When designing services in the NHS, there are invariably constraints involved. In the case of genetic testing, there is currently no integration between local hospital systems and the national lab infrastructure. This meant implementing a service with a paper form and returning results via email. The teams involved worked with their local IT teams to integrate with their local systems to ensure tests could still be ordered digitally - as per their current processes. We identified that integrating results with local IT systems is a key enabler for this testing to have an impact on patient care.
“As doctors and researchers, we are often overly focussed on the science and the detail; forgetting that innovation in healthcare is ultimately about improving people’s lives. Emma’s perspective has not just added value to the project but left a lasting impact on ways of thinking and problem solving.”
- Videha Sharma, Clinical Innovation Lead at University of Manchester NHS Foundation Trust
Testing and iterating parts of the service.
As part of this work we developed prototypes for key parts of the service like the test ordering form and the patient information leaflet. We tested these with the clinical staff and patients who would be using them and iterated them based on the findings from this research. We were able to successfully redesign the lab testing form away from the standard approach to best meet the needs of this service.
Informing future roll out and influencing strategy.
One of the outputs from this project was an implementation guide to inform the future roll out of this testing service in hospitals across the country. Recommendations were detailed across the end-to-end service, including learnings and changes implemented as part of the pilot period to ensure that hospitals looking to implement testing could build on the learnings from this work. We provided an as-is service blueprint for clinical teams to use as a starting point for their own service development.
This work also provided strategic recommendations for commissioners working at a national level. In partnership with the pilot sites, we developed a to-be service blueprint for the ideal service that demonstrated the barriers to scaling and the impact on day-to-day service delivery at a local level. This work is helping to inform the continuing development of the national strategy for pharmacogenomics and the national approach to commissioning the testing.
